Procedures: ACL Reconstruction And Meniscal Repairs
Anterior Cruciate Ligament (ACL) reconstruction
%20tear.jpg?width=400&height=301&name=Anterior-cruciate-ligament%20(ACL)%20tear.jpg)
After an ACL rupture, patients are encouraged to undergo a rehabilitation programme aimed to reduce their knee swelling, control their pain, and maintain good movement of the knee and muscle strength. Though uncommon, there have been cases of people functioning well without an ACL, even performing normal daily activities such as walking and gentle jogging.
Problems may begin to arise when these activities are heightened, often twisting and torqueing the knee. This is when an ACL-deficient knee becomes unstable and painful. The instability may also cause your meniscus to tear and strain other ligaments around the knee. If the symptoms worsen despite adequate rest and medication, it is advisable to seek help from an orthopaedic surgeon.
Often, we receive young patients undergoing ACL reconstruction surgery, and only requiring general anaesthetic (GA) for their surgery. Once they are under GA, an arthroscopic (keyhole) assessment of their injured knee will be performed to determine the problems in the knee. It is common to find concurrent meniscal or cartilage injuries in the knee which can also be resolved during the surgery.
%20assessment.jpg?width=250&name=an%20arthroscopic%20(keyhole)%20assessment.jpg)
How is ACL reconstruction performed?
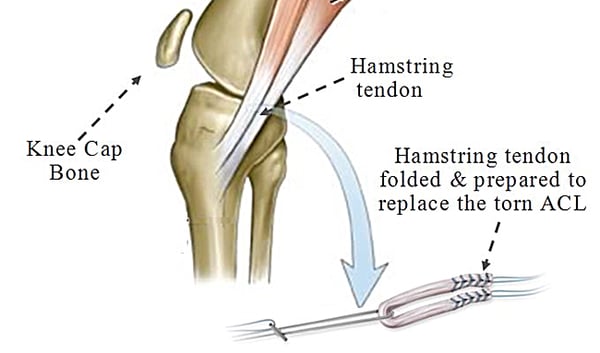
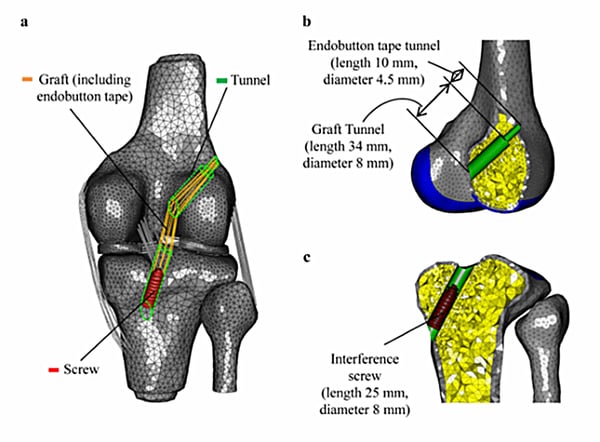
Part of the old ACL is shaven off using arthroscopic instruments, and the ACL will be reconstructed using the patient’s hamstring tendons. A small vertical incision is made to harvest their hamstrings from the same leg, which are folded to form a four-strand hamstring tendon graft. The hamstrings are then bound together with sutures to form a robust new ACL graft.
These techniques may work for some, but are associated with fractures of the patella and cause patella pain when patients kneel on the floor.
The ACL can also be reconstructed using two separate grafts through two separate bone tunnels through the tibia and femur each, but these carry a risk of fractures around the bone tunnels, causing the reconstruction to fail. Using an allograft (tissue from an organ donor) can also lead to a higher risk of rupture, especially in younger patients.
Ultimately, the use of hamstring tendons from the patient (autograft) and performing surgery through arthroscopic and minimally invasive techniques is a widely-adopted method, and a popular technique across the world.
What is the recovery like?
Phase 1
- To control pain and reduce the swelling in the knee
- Maintain the strength of your quadriceps tendon
- Early range of motion of the knee
Phase 2
- Improving the movement of your knee (extension and flexion)
- Removal of sutures
- Gait training and muscle strengthening
- Return to work
Phase 3
- To achieve a full range of motion of your knee
- Good strength in the operated knee, similar to the non-operated knee