Sports Knee Injuries
ACL Ruptures

What is an ACL?
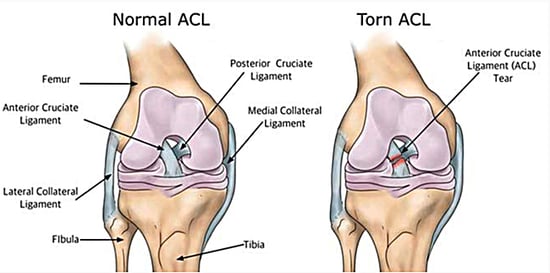
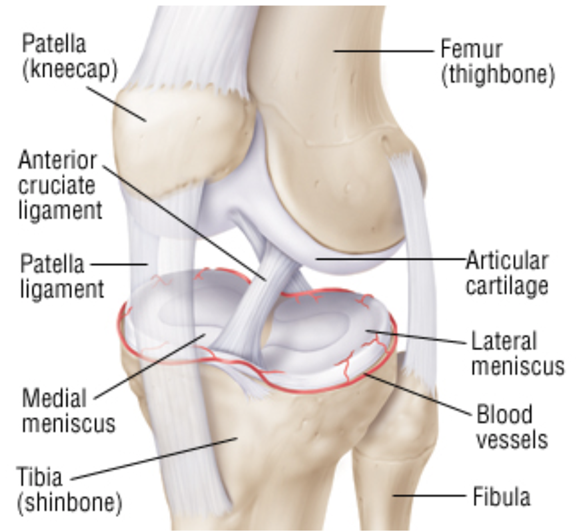
The anterior cruciate ligament connects two bones in your knees, the femur and tibia bones and gives the knee its rotational stability while controlling its back and forth movement. It allows you to do exercises that cause your knees to twist and turn. Without the ACL, your knee will feel unstable when doing activities such as basketball, football and tennis.
How does the ACL rupture?
The ACL is a rather strong and robust structure in the knee. However, it can still rupture in severe twisting injuries of the knee. An example is when a basketball player lands awkwardly and twists his or her knee. Footballers are also prone to this when the studs of their boots get stuck in the ground and they twist their body while running after the ball. This twisting injury of the knee while the foot is planted to the ground is enough to rupture the ACL. Several studies have shown that female athletes are at higher risk of ACL ruptures than their male counterparts due to differences in physical conditioning, muscular strength, effects of aestrogen and ligament laxity as well as anatomical differences in the pelvis and leg alignments.
How do I know if I ruptured my ACL?
Patients often have severe pain and swelling in the knee when they rupture their ACL. Some even report a ‘pop’ or snapping sound even before they hit the ground. After the initial period of pain and swelling, patients may experience stiffness or instability of their knee when performing certain activities. These include coming down the stairs, getting out of cars and playing sports that require twisting and turning (basketball, football). Patients may not get instability while jogging in a straight line or cycling as there is minimal twisting movement in the knee when performing these exercises. Oher symptoms include discomfort while walking, loss of range of motion and pain along the knee joint.
Your doctor will first take a thorough history from you about your injury, how you were immediately after the fall and what sorts of symptoms you get several weeks and months after the fall. A clinical examination of the knee is then performed to assess for knee swelling, general range of movement as well as stability of the knee. An x-ray of the knee will be done to exclude any fractures while an MRI would be the modality of choice to assess for an ACL rupture. Some patients have other injuries such as meniscal tears or ligament sprains in addition to the ACL rupture from the fall. The MRI scan of the knee will be able to pick up all these injuries in a single sitting.
Your doctor will first take a thorough history from you about your injury, how you were immediately after the fall and what sorts of symptoms you get several weeks and months after the fall. A clinical examination of the knee is then performed to assess for knee swelling, general range of movement as well as stability of the knee. An x-ray of the knee will be done to exclude any fractures while an MRI would be the modality of choice to assess for an ACL rupture. Some patients have other injuries such as meniscal tears or ligament sprains in addition to the ACL rupture from the fall. The MRI scan of the knee will be able to pick up all these injuries in a single sitting.
What treatments do I need after I rupture my ACL?
The initial aim of treatment is to reduce the pain and swelling in the knee. Anti-inflammatory medication, knee compression and ice packs are some of the ways we achieve this. A knee brace would be used to protect your knee from instability. To further protect you from falling, crutches may be provided to help you walk.
Physiotherapy after an ACL rupture is aimed at restroring normal range of motion of the knee, normal gait while walking and developing muscle strength of the quads and hamstring muscles. The torn or ruptured ACL will not heal itself. This is because the blood supply to the ACL had been disrupted during the injury itself.
Whether you decide to have surgery or not, rehabilitation plays a vital role in getting you back to you daily activities. Your surgeon and physiotherapist will customize a rehabilitation program for you to facilitate an accelerated recovery.
Physiotherapy after an ACL rupture is aimed at restroring normal range of motion of the knee, normal gait while walking and developing muscle strength of the quads and hamstring muscles. The torn or ruptured ACL will not heal itself. This is because the blood supply to the ACL had been disrupted during the injury itself.
Whether you decide to have surgery or not, rehabilitation plays a vital role in getting you back to you daily activities. Your surgeon and physiotherapist will customize a rehabilitation program for you to facilitate an accelerated recovery.
Can your ACL be repaired?
The ACL cannot be repaired after it has completely ruptured. Previous attempts at repairs by surgeons in the past were associated with severe knee pain and stiffness. Before any surgery is performed, your surgeon will ensure that the swelling in your knee has improved significantly, have a full range of motion and you should be able to walk normally on a flat surface.
The ACL must be reconstructed to restore the stability of your knee. This is done through arthroscopic or key-hole techniques to facilitate an early return to function. Your torn ACL is replaced with a tissue graft. There are several options to obtain this tissue graft including your own hamstrings, your patella and its surrounding tendons as well a cadaveric graft (allograft). There are advantages and disadvantages to all options. Your surgeon will discuss with you your best option.
The ACL must be reconstructed to restore the stability of your knee. This is done through arthroscopic or key-hole techniques to facilitate an early return to function. Your torn ACL is replaced with a tissue graft. There are several options to obtain this tissue graft including your own hamstrings, your patella and its surrounding tendons as well a cadaveric graft (allograft). There are advantages and disadvantages to all options. Your surgeon will discuss with you your best option.
ACL surgery and rehabilitation.
The ACL surgery itself takes about an hour to 90 minutes. Most patients are young and undergo this surgery under a general anaesthetic. There are two arthroscopic (less than 1cm) scars over the knee joint itself and another scar over the tibia where the hamstring is harvested from and the graft is advanced into the knee. A knee brace after surgery is crucial and is applied to provide some support and stability. Physiotherapy after surgery is aimed at reducing knee swelling and maintaining the strength of the quads muscle of your thigh. Both open and closed kinetic chain exercises are used to achieve full extension of your knee and about 70 degrees of flexion. At 3 to 4 weeks after surgery, you will improve on your walking with only one crutch and improve the control of your quads and hamstring muscles.
We will slowly wean you of the knee brace at about 5 weeks as your walking and muscle strength and control improves. At about 3 months, you will be allowed to perform exercises in a straight line such as running, jumping and cycling. These exercises will be varied in terms of duration, intensity, speed and complexity of tasks. The goal of rehabilitation at 4 to 5 months is to maximise endurance and strength of muscle around the knee. Strenuous twisting motion of the knee such as a return to football or basketball is not recommended before 12 months as your new ACL graft merely acts as a scaffold while your body adds new tissue to it and makes it strong again. There have been numerous examples of both social and professional athletes who returned to a high level of exercise and sports too early and re-ruptured their new ACL graft.
We will slowly wean you of the knee brace at about 5 weeks as your walking and muscle strength and control improves. At about 3 months, you will be allowed to perform exercises in a straight line such as running, jumping and cycling. These exercises will be varied in terms of duration, intensity, speed and complexity of tasks. The goal of rehabilitation at 4 to 5 months is to maximise endurance and strength of muscle around the knee. Strenuous twisting motion of the knee such as a return to football or basketball is not recommended before 12 months as your new ACL graft merely acts as a scaffold while your body adds new tissue to it and makes it strong again. There have been numerous examples of both social and professional athletes who returned to a high level of exercise and sports too early and re-ruptured their new ACL graft.
Meniscus injuries
What is the meniscus in the knee and what are they used for?
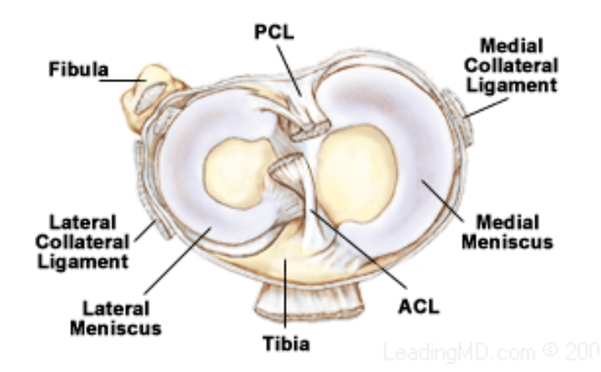
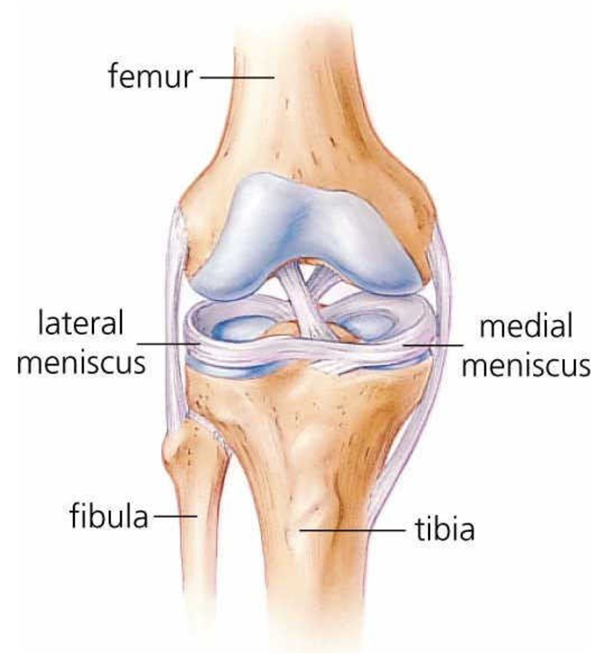
There are two menisci in each knee, the medial and lateral meniscus. They are c-shaped pieces of cartilage that function as a cushion or shock absorber between your femur and tibia bones. The menisci also provide some stability to your knee.
How do I know I have torn my meniscus?
Severe twisting injuries to your knee while weight is applied to it may lead to a torn meniscus. A torn meniscus leads to knee swelling, pain and stiffness. If it is a large tear, the displaced fragment of meniscus may jam your knee and prevent you from fully straightening or bending your knee (knee locking).
What can I do about it?
Pain and swelling of the knee may be managed by taking anti-inflammatory medication, knee compression as well as ice packs. Do seek the advice of an orthopaedic surgeon regarding your knee symptoms. He will take a detailed history from you, conduct a thorough clinical examination before arranging an xray and MRI of your knee. The MRI scan will assess the location and severity of the meniscal injury, as well as exclude other injuries to the knee. For minor meniscal tears around the periphery, conservative management with rest, time, anti-inflammatory medication and ice packs may help with the pain and swelling.
Surgery and recovery after meniscal surgery
Meniscal repair surgery is performed through key-hole skin incisions measuring less than 1cm each. The meniscus receives its blood supply from its periphery. As such, simple or linear tears around the periphery have a better chance of healing with surgical repair compared to tears on the inner surface of the meniscus. Tears in the inner surface (white white zone) of the meniscus are trimmed to prevent it from getting bigger.
After surgery, your knee will be protected in a knee brace and your surgeon may restrict how much you bend your knee to allow the meniscus to heal. Physiotherapy and rehabilitation after surgery are aimed at reducing pain and swelling of the knee, as well as strengthen the quads and hamstrings muscles around the knee.
After surgery, your knee will be protected in a knee brace and your surgeon may restrict how much you bend your knee to allow the meniscus to heal. Physiotherapy and rehabilitation after surgery are aimed at reducing pain and swelling of the knee, as well as strengthen the quads and hamstrings muscles around the knee.
Runners’ Knee
Pain around the knee does not only happen to runners but to any one of us while we carry out our daily activities. Knee pain may also be in the front, sides or all across the knee. Your orthopaedic surgeon will take a detailed history to determine the type of activities which aggravate your knee pain and performed a thorough clinical examination to determine which part of your knee is actually hurting.
Common causes of knee pain include muscle imbalance and overuse activities like lunges, squats and jumps. Weak quadriceps muscles of the thigh may cause the patella to be pulled in the wrong direction as the knee is straightened and flexed. Your orthopaedic surgeon and physiotherapist will customize a rehabilitation program to strengthen the quadriceps muscles of your thigh and improve the pull of the patella. Despite your knee hurting, it may be your feet causing the symptoms. Patients with flat feet or over-pronated feet are unable to support their knee the way they should. Excessive stress around the knee will cause knee pain with simple daily activities. Your orthopaedic surgeon will assess your feet and both legs for any problems of malalignment. Insoles may be used to correct problems with flat feet.
Chondromalacia patella is a condition where the cartilage under the patella breaks down. After a thorough clinical examination by your orthopaedic surgeon, an MRI scan of your knee will be done to assess the cartilage under the patella.. There is evidence to show that intra-articular injections such as platelet rich protein (PRP) and viscosupplementation are effective in reducing pain and improving function in patients with arthritic knee pain.
Common causes of knee pain include muscle imbalance and overuse activities like lunges, squats and jumps. Weak quadriceps muscles of the thigh may cause the patella to be pulled in the wrong direction as the knee is straightened and flexed. Your orthopaedic surgeon and physiotherapist will customize a rehabilitation program to strengthen the quadriceps muscles of your thigh and improve the pull of the patella. Despite your knee hurting, it may be your feet causing the symptoms. Patients with flat feet or over-pronated feet are unable to support their knee the way they should. Excessive stress around the knee will cause knee pain with simple daily activities. Your orthopaedic surgeon will assess your feet and both legs for any problems of malalignment. Insoles may be used to correct problems with flat feet.
Chondromalacia patella is a condition where the cartilage under the patella breaks down. After a thorough clinical examination by your orthopaedic surgeon, an MRI scan of your knee will be done to assess the cartilage under the patella.. There is evidence to show that intra-articular injections such as platelet rich protein (PRP) and viscosupplementation are effective in reducing pain and improving function in patients with arthritic knee pain.