Conditions
Types of Knee Arthritis

Arthritis is when a joint (like your knee) gets inflamed, which can cause pain, stiffness, and swelling. There are a few main types that affect the knee, and each works a little differently.
- Osteoarthritis (OA) – "Wear and Tear" Arthritis
Osteoarthritis is the most common type of arthritis. It’s often called “wear and tear” arthritis because it happens when the cartilage in your joints wears down over time. Cartilage is the smooth, rubbery stuff that covers the ends of bones and helps your joints move easily.
When it wears away, bones start to rub against each other — and that’s when the pain, swelling, and stiffness begin. Mostly adults over 40, but younger people can get it too — especially after joint injuries (like ACL tears or fractures). OA is more common in women and people with family history of arthritis.
- Joint pain – especially after activity or at the end of the day
- Stiffness – usually after resting or waking up
- Swelling – the joint may look a little puffy
- Popping or grinding sounds (called crepitus)
- Less movement – the joint may not move as easily as before
It most often affects the knees, hips, fingers, lower back, and neck.
2. Rheumatoid Arthritis (RA) – "Immune System" Arthritis
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes inflammation in the joints, leading to pain, swelling, stiffness, and potential joint damage. It's characterized by the immune system mistakenly attacking the joint lining, a layer of tissue called the synovium. RA often affects multiple joints symmetrically, meaning both sides of the body are typically affected at the same time eg both knees, wrists or hands. If left untreated, RA can cause significant joint damage, leadig to bone and cartilage destruction. RA may also affect other parts of the body such as the eyes, skin, heart, lungs and blood vessels. While there is no cure for RA, early diagnosis and treatment with medication can slow the disease progression and prevent long term joint damage.
- Stiff joints in the morning (lasting longer than 30–60 minutes)
- Swollen, tender joints – usually in a symmetric pattern (both sides of the body)
- Fatigue – you may feel super tired, even if you slept
- Low-grade fever
- Weight loss or loss of appetite (in some cases)
It often starts slowly but can become more serious over time if untreated.
3. Psoriatic Arthritis - "Immune System" Arthritis
Similar to RA, Psoriatic arthritis is an autoimmune disease where the immune system gets confused and attackes your own joints causing pain and swelling. It affects patients with psoriasis, a skin disease characterised by patches of thick, red skin with silvery-white scales that itch or burn, typically on the elbows, knees, scalp, trunk, palms, and soles of the feet. While not everyone with psoriasis develops arthritis, about 1 in 3 people with psoriasis do.
• Joint pain and stiffness – often in the knees, fingers, toes, or spine
• Swelling – joints may look puffy or sausage-like (especially fingers/toes)
• Fatigue – feeling really tired is common
• Morning stiffness – joints feel stiff after waking up
• Skin and nails – psoriasis patches on the skin; nails may be pitted or crumbly
4. Gout – "Crystal" Arthritis
Gout or crystal arthritis is a type of arthritis that happens when uric acid builds up in the blood and forms sharp crystals in the joints. Normally, uric acid is eliminated through urine, but if your body produces too much or doesn't get rid of enough, the uric acid builds up in your bloodstream. This extra uric acid can form needle-like crystals that settle in your joints, causing sudden, severe pain, swelling, and redness in the affected area, usually starting in the big toe but can affect other joints too (like the knee or ankle). Sudden attacks of pain, often at night
• Intense joint pain – usually in the big toe (but can also affect the ankle, knee, or fingers)
• Red, swollen, and hot joint – looks inflamed and feels warm to the touch
• Pain often starts suddenly, usually at night
• Limited movement – you might not be able to move the affected joint due to pain
A gout attack can last for hours or days, and it often comes and goes in "episodes" (flare-ups).
5. Post-Traumatic Arthritis
Post-traumatic arthritis is a type of arthritis that happens after a joint injury — like a fracture (broken bone), ligament tear, or cartilage damage. It can affect any joint, but it’s especially common in the knees, ankles, and shoulders. The injury doesn’t have to be huge — even smaller injuries, over time, can lead to joint damage that causes pain, swelling, and stiffness.
When a joint is injured, it doesn’t always heal perfectly. That damage can wear down the cartilage (the smooth layer that helps your joints move easily). Over time, this wear and tear can lead to arthritis, even months or years after the injury.
Injury → Joint damage → Wear & tear → Arthritis symptoms
- Pain in the injured joint (especially during or after activity)
- Swelling or stiffness in the joint
- Limited movement or “tight” feeling
- Grinding or clicking feeling in the joint
Pain that gets worse over time
How is knee arthritis diagnosed?
Clinical history and examinationYour doctor will take a detailed history about your knee pain. Questions include duration and severity of pain, character and nature of pain such as whether it happens all the time and what makes it worse. The doctor will also ask other associated symptoms such as knee swelling or instability, fever, any skin lesions or other joint involvement. A history of falls, trauma or infection may also be relevant.
Once the history taking is completed, the doctor will assess your walking gait, looking for a limp, the smoothness of the gait and if there are any malalignments or deformities of your leg. You will then be asked to lie down on the examination couch where a thorough examination of both knees will be done. This is to assess for pain, swelling, range of motion and stability of the knee. If needed, the doctor may also examine both your hips and ankles to ensure that the knee pain is not coming from a different joint altogether.
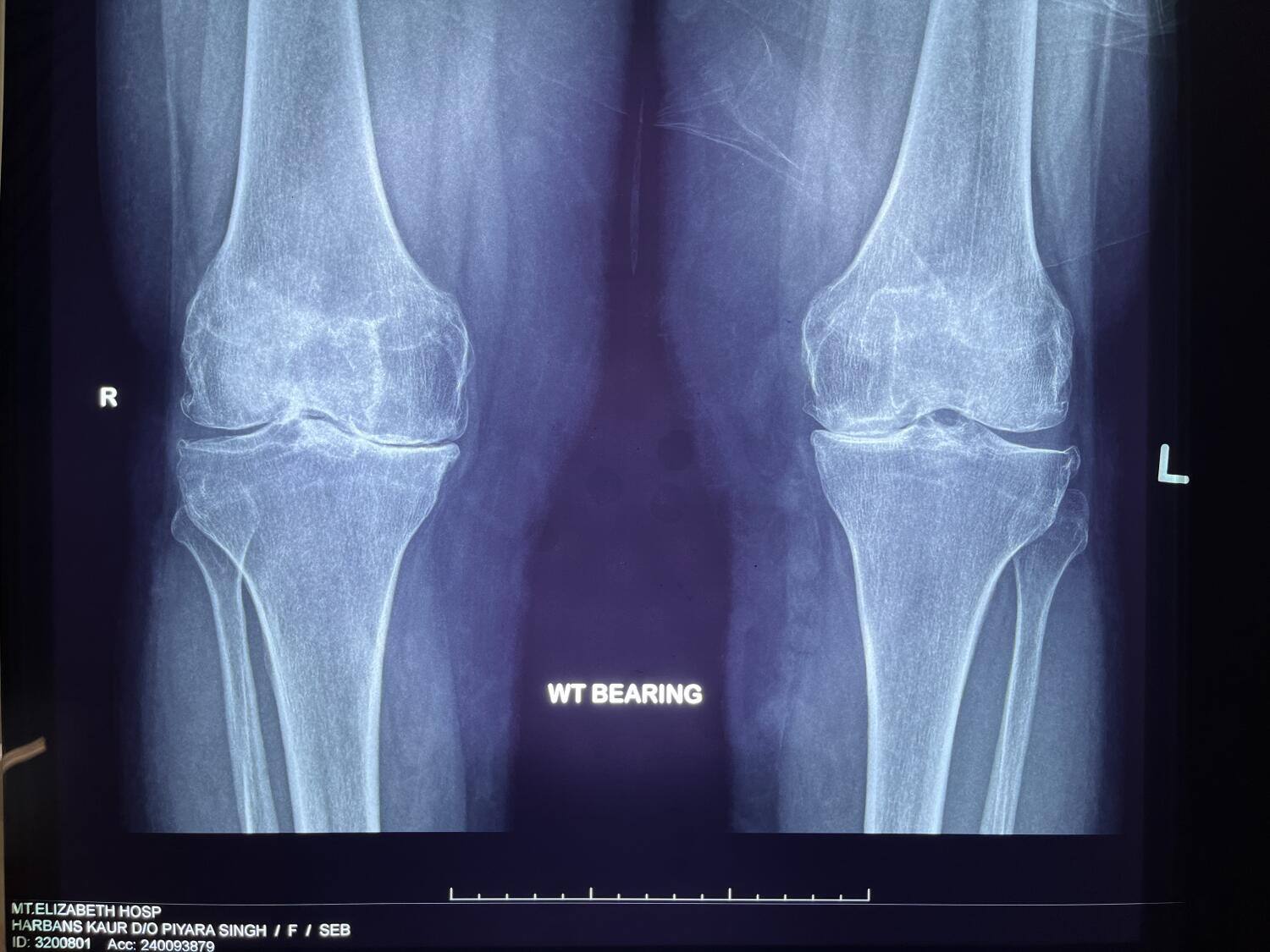
It is common to have x-ray images of both knees while you are standing. X-rays show the general alignment of the lower limb as well as the bony architecture of the knee joint. Weight bearing images are useful as it allows any reduction in your joint space to be picked up. This may indicate arthritis in your knee joint.

Weight bearing views from the front shows bone on bone contact in the medial compartment of the left knee.
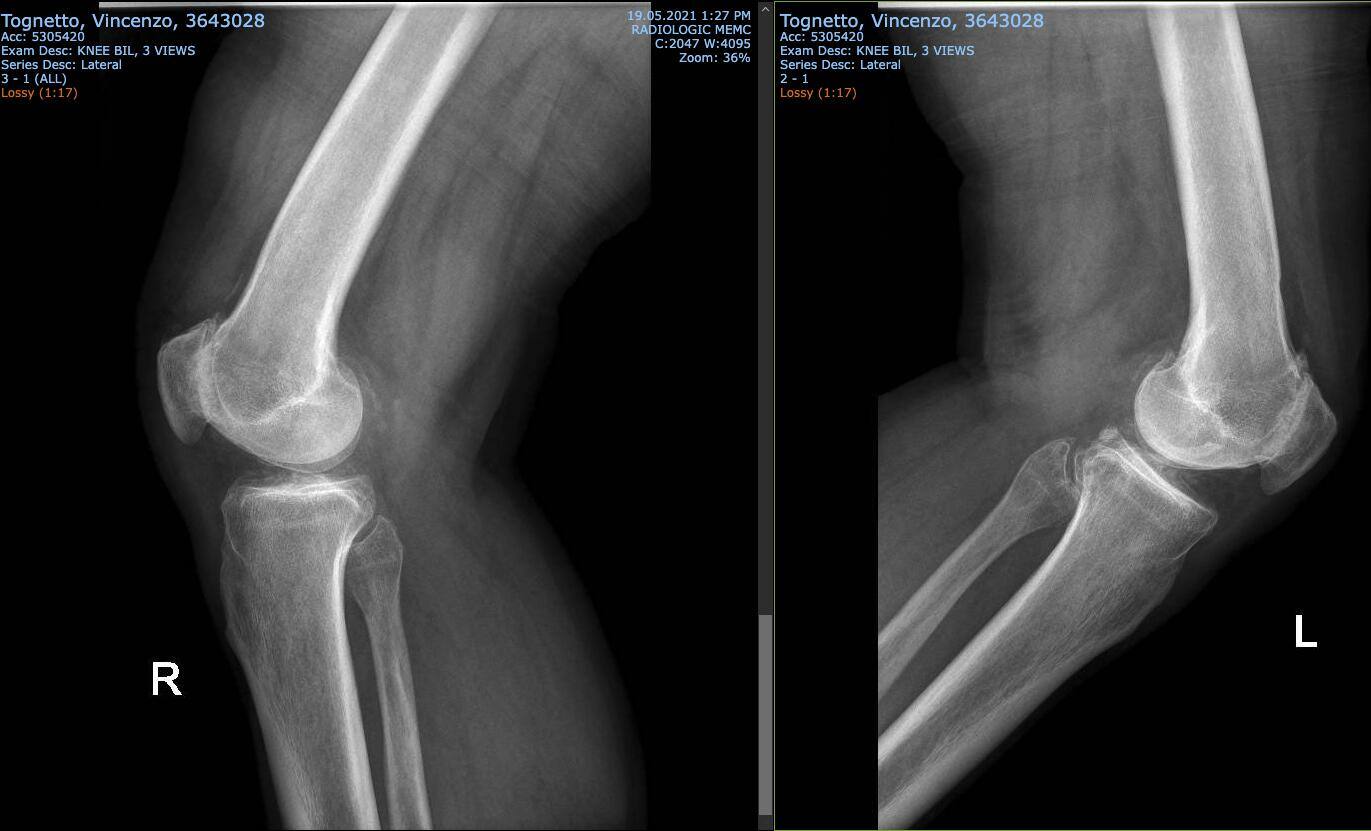
Side or lateral views of both knees show the relationship between the patella and femur. They also show up any bone spurs at the back of the knee
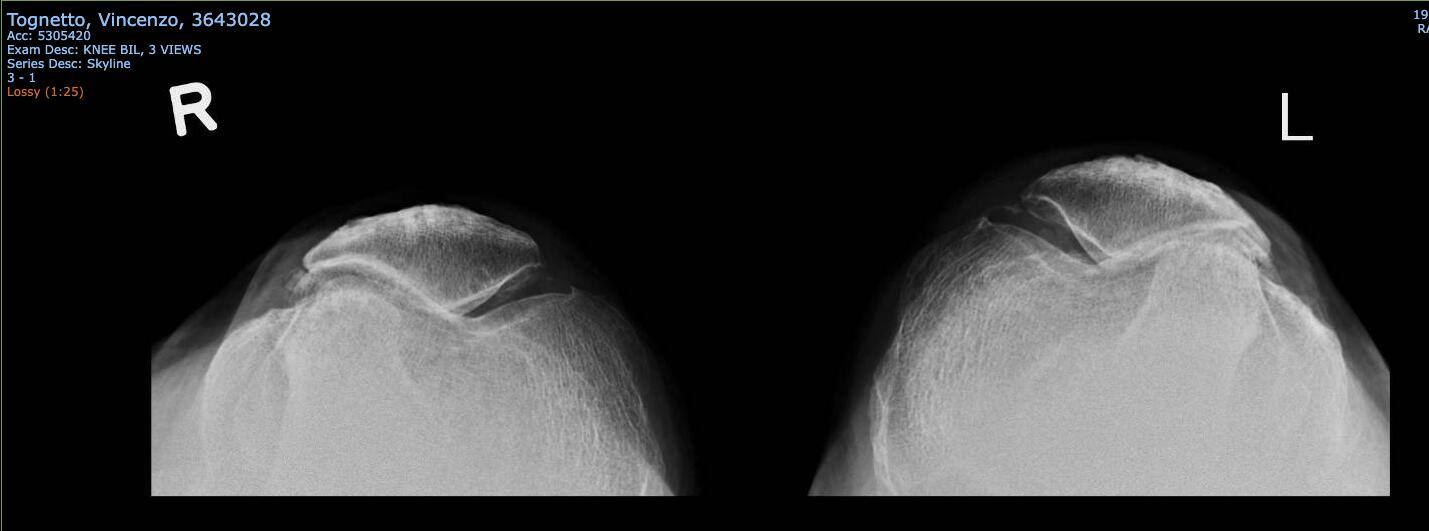
The skyline view of the knee illustrates the loss of joint space between the patella and the femur, as well as the lateralization or lateral tracking of the patella.
In younger patients or those whose x-ray images are inconclusive, an MRI scan is helpful to assess for soft tissue injuries. These soft tissue structures include cartilage, meniscus, ligaments as well as synovial tissue. The MRI images include all three compartments of the knee including the back of the knee.
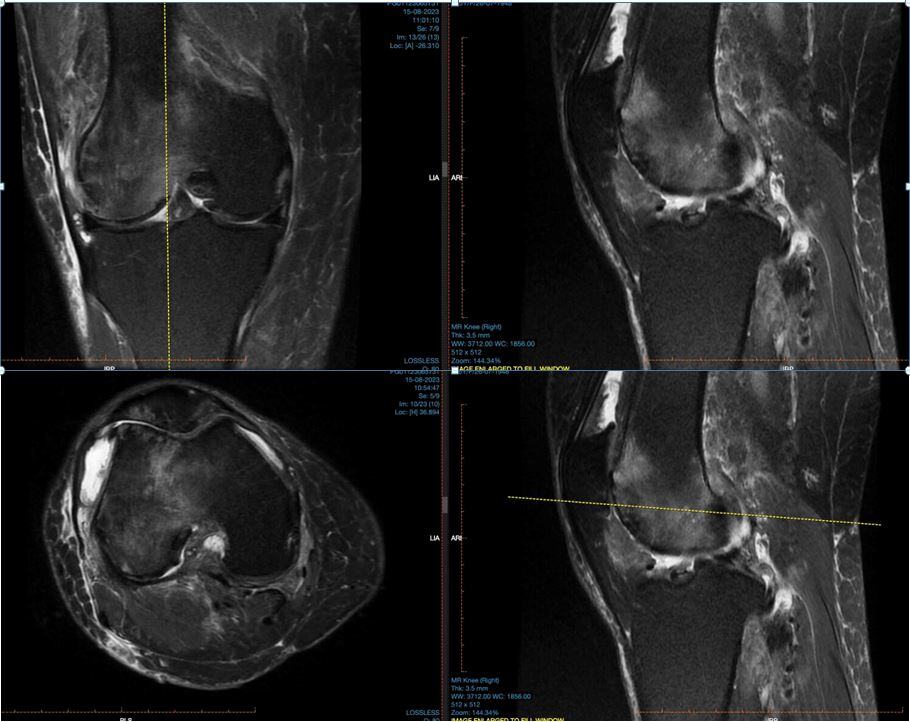
MRI images show degeneration of soft tissue as well as swelling/oedema of bones. These internal injuries reflect the amount of pain patients experience from their knee arthritis.
Blood tests
Basic blood tests may include your full blood count, white cell count and kidney function.
Additional blood test may look for gout (raised uric acid), Rheumatoid arthritis (rheumatoid factor, ESR) and infection (CRP).
Treatment options for Knee Osteoarthritis
1. Stay Active (But Smart!)
Exercise is one of the best things you can do for knee OA. It might sound strange, but moving your knee is one of the best things you can do. It keeps the joint flexible and the muscles strong.
- Low-impact exercises like walking, swimming, cycling, or yoga help keep your joints moving without too much stress.
- Strength training (especially for your thighs and hips) supports your knee and reduces pain. Focus on building muscle around your knee — especially your thighs (quads and hamstrings). Strong muscles = better knee support.
- Stretching improves flexibility and helps with stiffness.
💡 Tip: Even 20–30 minutes a day makes a difference!
2. Keep a Healthy Weight
If you're carrying extra weight, it puts more pressure on your knees. Losing even a little (5–10% of your body weight) can reduce pain and slow down the damage. Weight loss is not all about exercise. Managing a healthy diet with high protein, vegetables and fruits and a lower amount of process foods, sugar and carbohydrates will help you reach your ideal weight. Hydration is also a very important aspect of good nutrition and health.
3. Hot & Cold Therapy
- Ice packs applied around the knees help to reduce swelling and pain after activity. They allow joints to recover faster from inflammation. This will allow you to engage in more regular aerobic and low impact exercises as well as avoid injuries to the knee.
- Warm compresses or baths relax stiff joints and muscles. You may enjoy them before or after exercise.
4. Medications
These help manage pain and inflammation so that you may continue to lead an active lifestyle
- NSAIDs (like ibuprofen or naproxen) – for pain and joint swelling
- Acetaminophen (Paracetamol) – for pain (if you can’t take NSAIDs)
- Topical creams – rubbed on the knee for local relief
5. Injections
Sometimes the knee pain may be moderate to severe and it holds you back from being active. Do check with your doctor first if there are any serious injuries in your knee such as a torn meniscus or ligaments. In patients with general wear and tear of their cartilage, injections may help reduce the pain and smoothen their knee range of motion.
- Types of knee injections:
- Corticosteroids – reduce inflammation during flare-ups
- Hyaluronic acid – adds lubrication to the joint (results vary)
- Blood – helps reduce inflammatory cytokines in your knee which cause your cartilage to be soft and vulnerable. Also helps soft tissue recover.
Your doctor will ensure the skin in cleaned first with an antiseptic before applying a small dose of local anaesthetic to the skin over the knee. After a few minutes, the doctor will then administer the hyaluronic acid and/or steroid injection into your knee. A plaster will be applied and you are allowed to walk on your knee immediately after the injection. You do not need crutches or a brace after a knee injection.
6. Supportive Gear
The right gear can reduce strain and help you move easier.
- Knee braces or sleeves: Provide support and reduce pain during activity.
- Orthotic shoe inserts: Help with balance and take pressure off the joint.
- Walking aids (if needed): A cane or hiking pole can reduce stress on the knee during long walks or rough terrain.
7. Physiotherapy and Physical Therapy
A physiotherapist (PT) is a trained movement expert who creates a plan just for you. They will:
- Assess how your knee moves and how strong your muscles are
- Teach you safe, joint-friendly exercises
- Help correct posture and walking habits
- Use hands-on techniques (sometimes) like massage or mobilization
- Use equipment such as shockwave therapy or ultrasound therapy to help accelerate the recovery of your knee
- Give tips for protecting your knees during daily activities
Key Parts of a Physio Program
1. Strengthening Exercises
These build muscles that support and protect your knee — especially your quads, hamstrings, glutes, and calves.
Examples:
- Straight leg raises
- Wall sits
- Step-ups
- Resistance band knee extensions
2. Stretching & Flexibility
Stiff joints hurt more. Gentle stretches help you move better and reduce tightness.
Examples:
- Hamstring stretch
- Calf stretch
- Quad stretch
- Knee-to-chest stretch (lying down)
3. Balance & Coordination Work
Knee arthritis can affect your stability. PTs use balance training to reduce the risk of falls or awkward movements.
🟢 Examples:
- Standing on one leg
- Heel-to-toe walk
- Stability ball exercises
4. Low-Impact Cardio
Keeps your joints moving and your heart healthy.
🟢 Safe options:
- Stationary biking
- Swimming or water aerobics
- Elliptical trainer
- Walking on flat surfaces
Do They Use Other Treatments?
Some PT clinics may offer:
- Heat or ice therapy
- Ultrasound or electrical stimulation (TENS)
- Shockwave therapy
- Taping or bracing
- Dry needling or massage therapy
These can support your progress but are usually used with exercise, not instead of it.
💡 Bonus Tips from Physios
- Don’t push through sharp pain. Some discomfort is normal, but sharp pain = stop.
- Keep moving every day. Even 10 minutes of movement is better than none.
- Stick to your home exercises. PT works best when you stay consistent.
- Track your progress. Improvements can be small at first — don’t get discouraged!
8. Surgical Procedures for pain
There are lots of patients who may continue to experience some level of pain or discomfort despite various conservative treatment modalities. They may need more pain relief to support their busy lives but cannot afford any downtime associated with surgery.
This group of patient may benefit from a pain procedure to reduce their knee pain without actually addressing their knee arthritis itself. There are very specific pain or nociceptive fibres and nerves around the knee. Nociceptors, the nerve endings of nociceptive fibers, are located in the skin, muscles, joints, and internal organs. They act as sensors, detecting noxious stimuli and converting them into electrical signals that travel along the nociceptive fibers to the central nervous system. Nociceptive pain plays a vital role in protecting the body from further injury by alerting us to potential harm. However, in certain conditions, such as chronic pain, nociceptive pathways can become sensitized, leading to heightened pain sensitivity and the perception of pain in the absence of a noxious stimulus.
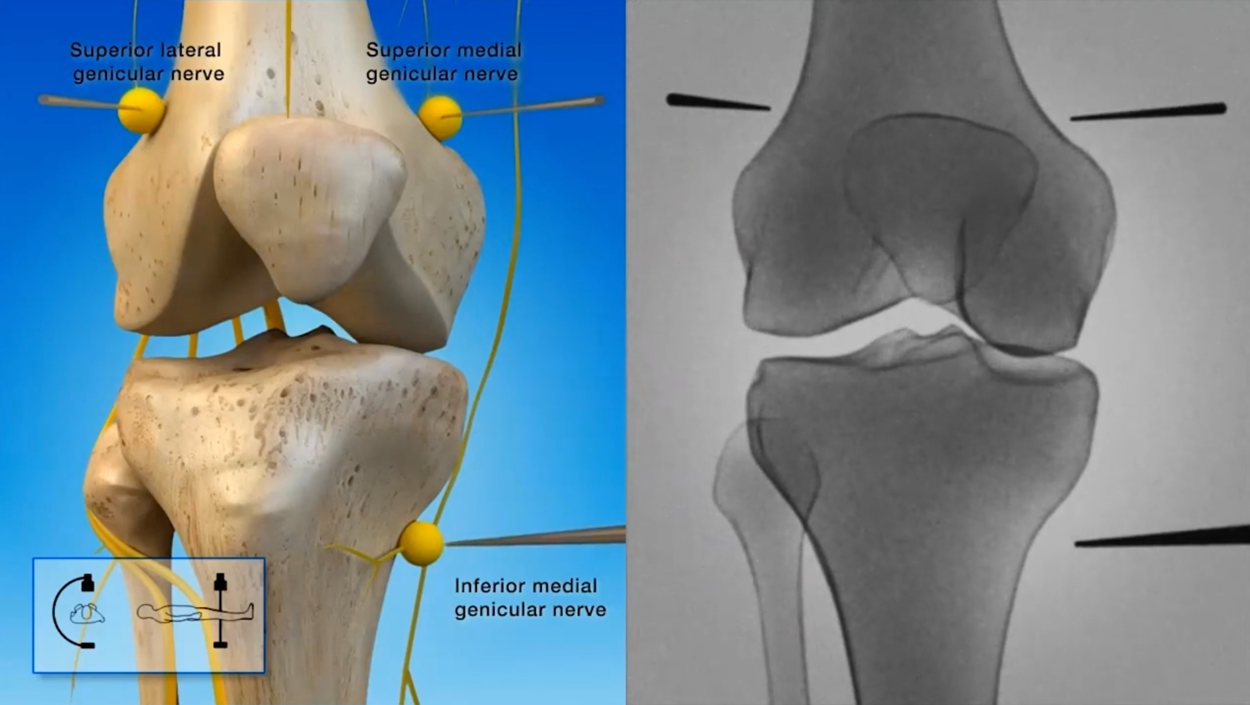
Orthopaedic surgeons and pain physicians (anaesthetists) often carrying out a procedure called radiofrequency ablation of nociceptive or pain fibres to help manage knee pain. This procedure helps to bridge the gap between short-term pain relief treatments and knee surgery by providing a minimally invasive, non-opioid procedure for OA knee pain. Needles are strategically placed through the skin towards three specific nerves under either x-ray or ultrasound guidance. Once their exact positions have been confirmed, heat is applied to the nerves to ablate or burn away the sensitised nerve fibres. This helps to patients experience significantly less pain and may last up to two years.
Do speak to your surgeon to see if this is an appropriate procedure for you.
9. Surgeries for knee osteoarthritis
- Arthroscopy (Minimally Invasive /Key-hole0
A tiny camera and tools are inserted through small cuts to “clean out” the joint.
- Cartilage injuries: Cartilage ulcers may be debrided if they are too worn out. However most patients will benefit from cartilage repair and regeneration through a process of nanofracture. This allows blood from patients bone marrow to develop into new hyaline-like cartilage or fibrocartilage. This new layer of cartilage may not be as sturdy and thick as your original hyaline cartilage but some cartilage is better than none.
- If there are any meniscus tears found in your knee, your surgeon will decide whether to debride it or repair it with sutures to maintain its integrity./ Meniscus are important shock absorbers of the knee which protect the knee cartilage.
- Works best for mild OA or injuries — not great for advanced OA
✅ Pros: Quick recovery, small scars
❌ Cons: Doesn’t fix deeper joint damage, benefits may not last long
- Osteotomy (Bone Realignment Surgery)
This surgery reshapes or realigns bones to take pressure off the damaged part of the joint. Some patient have misaligned knees and this causes excessive pressure and load to specific parts of the knee. The overloaded part of the knee experiences accelerated wear and tear as well as pain. Osteotomies or bone realignment surgery is aimed at offloaded the painful part of the knee so that patients experience less pain. This is a form of knee preservation surgery and helps to delay knee replacement surgery.
- Often used for younger, active people with knee OA in just one area
- Bone is cut and repositioned to shift your weight to a healthier part of the joint
✅ Pros: Can delay need for joint replacement
❌ Cons: Longer recovery, not suitable for advanced OA

- Partial Joint Replacement (Unicompartmental Replacement)
Only the damaged part of the joint (usually one side of the knee) is replaced with a metal and plastic part. It leaves the other two compartments of the knee alone. This procedure is appropriate for younger and more active patients. Patients are informed that if other parts of their knee wears out over time, the partial knee replacement may need to be converted to a total knee replacement in future. This involves a second operation.
- Less invasive than full replacement
- Keeps more of your natural joint
✅ Pros: Shorter surgery, quicker recovery
❌ Cons: Only works if damage is limited to one area


A right knee before and after a partial knee replacement. Other than the obvious implant, do note the knee is straighter after the surgery compared to a slight varus deformity before surgery.
4. Total Joint Replacement (Arthroplasty)
This is the most common and most effective surgery for severe OA. It replaces all worn out cartilage and meniscus in your knee. Where patients have severe deformities of their knee, the orthopaedic surgeon is able to restore stable alignment of your knee through the knee replacement procedure. Even the worn on cartilage on your patella (knee cap) can be replaced. This is the most common joint replacement procedure in the world and helps patients regain their active and healthy lifestyles.
- Entire joint is replaced with an artificial one (metal and plastic parts).
- Arthritis and malalignment are both addressed through one surgery
- Patients are allowed to full weight bear after surgery and start physiotherapy early.
- Most patients will require a walking aid for a few weeks before they can walk on their own. Each patient is different so post operative function is very dependenton each patients general health and fitness.
- The vast majority of patients who have knee joint replacements are 55 years old and older. Most of them will not need any further surgery in their lives as more than 95% of implants do not require any revision surgery after 15–20+ years. Only about 5% of patients may require revision surgery in future from loosening or wearing out of implants.


Typical x-rays of both knees showing significant wear and tear over the medial knee joint. The femur and tibia bones are touching each other and there is no medial joint space to speak off. There are also bone spurs or osteophytes which confirm the diagnosis of knee osteoarthritis.

Post-operative x-rays showing implants over the femur, tibia as well as the patella
What to Expect After Surgery
- Physical and physiotherapy are a huge part of recovery and rehabilitation.
- You’ll slowly regain strength, flexibility, and confidence in your joint
- Full recovery can take several months, this depends on many factors such as body habitus, underlying physical fitness or lack of, pain threshold, frailty and many others. There will be many milestones to achieve during that period. They include walking without a walking stick, getting smooth walking gait, able to walk up stairs one foot at a time, not require pain killers and getting on with your daily activities without having to think about your knee!
- Physiotherapy can even start the day of your surgery! Your trainer will help you on your feet with the use of a walking frame and start taking your first steps around your hospital bed. For those who are doing well, you may walk along the hospital corridor.
Timeline of post-surgery rehabilitation:
- Day 1-2: Gentle movements to prevent stiffness.
- Week 1-2: Light range-of-motion and strengthening exercises.
- Week 3-6: Progressive weight-bearing and strength-building.
- Week 6 and beyond: Advanced mobility and balance training.
Importance of consulting a physical therapist
- Precautions Before Starting Exercise
- Recognising pain versus normal discomfort.
- Avoiding overexertion and improper techniques.
- Signs to stop or modify an exercise (e.g., swelling, sharp pain).
Early-Stage Exercises (First Few Days Post-Surgery)
- Ankle Pumps & Circles: Prevents blood clots and improves circulation.
- Quadriceps Sets: Strengthens the thigh muscles without moving the knee.
- Heel Slides: Helps regain knee flexibility.
- Seated & Lying Down Exercises (Week 1-2)
- Leg Raises: Builds quadriceps strength without excessive knee movement.
- Knee Extension Stretch: Helps fully straighten the knee.
- Hamstring Stretch: Improves flexibility in the back of the leg.
- Standing & Weight-Bearing Exercises (Week 3-6)
- Mini Squats: Strengthens the thighs and enhances knee stability.
- Step-Ups: Helps with stair climbing and mobility.
- Heel and Toe Raises: Strengthens the calf muscles and improves balance.
Advanced Strengthening & Mobility Exercises (Week 6 and Beyond)
- Stationary Cycling: Improves knee flexibility and builds endurance.
- Resistance Band Exercises: Strengthens surrounding muscles.
- Balance Training: Helps improve coordination and prevents falls.
- Water-Based Exercises for Gentle Strengthening
- Pool Walking: Reduces joint impact while promoting movement.
- Aqua Leg Lifts: Strengthens muscles with minimal strain.
Common Mistakes to Avoid During Recovery
- Overexerting too soon and risking injury.
- Skipping exercises due to discomfort.
- Using improper form, leading to poor recovery outcomes.
How to Track Your Progress
- Monitoring pain levels, flexibility, and strength improvements.
- Setting small, achievable recovery goals.
- You will notice that you require much less medication, stopped using your wakling aids and walk or climb stairs much smoother with less effort. Soon you will have forgotten you even had a knee replacement! Book a short holiday about 3 or 4 months after surgery which will serve as further motivation to get better!
FAQs on Knee Replacement Recovery Exercises
- How soon can I walk without a walker?
You can start walking on the day of surgery itself if you do not feel dizzy or light headed. If your surgery ended late in the evening, you may start walking the following morning. - Can I kneel after a knee replacement?
For patients to be able to knee, they should be able to bend their knee 90 degrees or more. How much patients can bend their knees depends on their knee stiffness BEFORE surgery, type of knee replacement they underwent, girth of their thigh and calf as well as the physiotherapy they received after surgery. Some people are able to kneel and bend their knee but are worried that they do not have enough strength in the legs to get up after that. Hence the importance of physical therapy after surgery to help you achieve all these goals! - What exercises should I avoid permanently?
Non or low impact physical and sporting activities are highly encouraged after knee replacement surgery. It helps keep a healthy and fit body without putting too much repetitive stress on the knee and implants. Activities such as cycling, swimming, walking and aerobic exercises are great for everyone. Long distance running, regular heavy weight lifting and pivoting sports like football are not encouraged as unexpected injuries may cause fractures around the knee and loosening of the implants.
Conclusion
Knee arthritis is a common condition affecting even the healthiest and fittest of us. It is first important to identify and diagnose it before appropriate and effective treatment may be administered. Most conservative techniques are effective but invasive options such as injections, key hole surgery may be required in some patients. Partial and total knee replacements are good surgical options for patients with advanced arthritis. All these techniques are aimed at keeping you fit and active throughout your life. Do seek medical assistance if you think you may be suffering from knee arthritis.