What You Need To Know After Your Hip Replacement Surgery
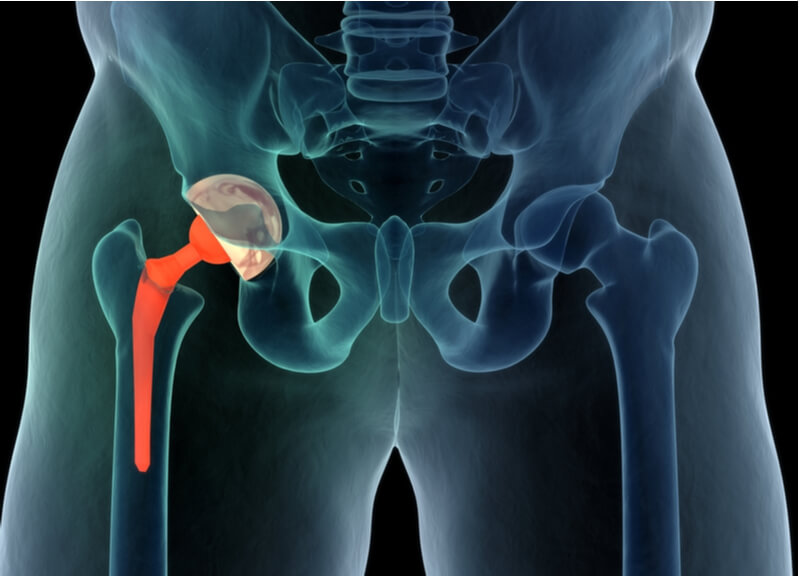
What exactly is a total hip replacement?
A Total Hip replacement (THR) is a surgical procedure to remove the worn out parts of the hip (femur and acetabulum) with implants. It is often performed for patients with hip arthritis. While there are a variety of reasons why patients may require a THR, most patients would have been experiencing hip pain, stiffness, difficulty walking and even a leg length discrepancy for some time before requiring a THR.
When patients present with hip symptoms, their orthopaedic surgeon will take a thorough history and perform a clinical examination to identify the location of the pain and the cause of the problem. Initial imaging using X-rays will be taken for both hips from the front and side profiles to confirm the diagnosis of hip arthritis. Depending on the severity of the condition itself, conservative management using medication, physiotherapy and activity modification may be used before surgery is considered.
Who would benefit from a Total Hip Replacement?
There are several reasons why patients suffer from severe and persistent hip pain. The most common cause is osteoarthritis, where there is age related and activity related wear and tear of the hip joint itself.
Inflammatory arthritis such as Rheumatoid Arthritis, Gout and Ankylosing Spondylitis are an autoimmune condition where the immune system malfunctions and mistakenly attacks healthy tissues and organs. Patients with inflammatory arthritis may experience earlier onset hip arthritis with their hips wearing out in their 30’s or 40’s.
Another group of patients who may experience early hip arthritis are those suffering from Avascular Necrosis (AVN) of their hips. The blood supply to the hip joint is compromised causing the femur bone to die from a lack of blood supply. The common causes of AVN include excessive alcohol, prolonged steroid use, chemotherapy medication, previous trauma and infection of the hip. There are other less common causes of hip AVN.
Regardless of the actual cause of their hips wearing out, patients experience deteriorating quality of life due to pain, stiffness and loss of function. The psychological and mental aspect of chronic hip pain also plays a part in patients becoming more withdrawn and reducing social interactions with family members and friends as they do not want to be a burden to others. Some are embarrassed by their limp or walking gait and may decline going for walks which they once used to enjoy.
Why should you have a total hip replacement?
Patients diagnosed with arthritis may find their condition worsening despite medication, physiotherapy and modifying their daily and sporting activities. When the cushioning effects of cartilage over the femoral head and acetabulum are lost, the stress from patients’ body weight causes painful bone to bone contact causing severe and persistent pain. Loss of cartilage also leads to shortening of the leg, causing patients to limp form pain and the limb length discrepancy. At this point, patients should strongly consider a total hip replacement and discuss this in great detail with their orthopaedic surgeon.
The THR is aimed at replacing only the parts that are worn out so that patients may continue to be active, mobile and live out their dreams and aspiration. It allows patients to exercise, enjoy their hobbies as well as the simple things in life like walks in the park, hiking, swimming and biking.
I often explain to my patients that you should enjoy a good quality of life now, and not only when you’re 60 years old and above and retired. The quality of implants manufacturing and surgical techniques have certainly improved significantly to allow patients to have this hip replacement procedure even when they’re in their 30’s or 40’s.
How is a Hip Replacement performed?
Patients may undergo a THR either under general anaesthetic or through regional anaesthesia. Depending on surgeon’s preference and surgical experience, orthopaedic surgeons may place patients on their side during surgery or on their backs for patients have the THR through the direct anterior approach. Before any skin incision is made, patients receive prophylactic intravenous antibiotics to prevent any infection from setting in. The surgical side is then cleaned thoroughly with anti-septic solution before they are covered with sterile drapes.
Once the surgical incision has been made and the orthopaedic surgeons exposes the actual hip joint, he proceeds to remove the worn out femoral head.
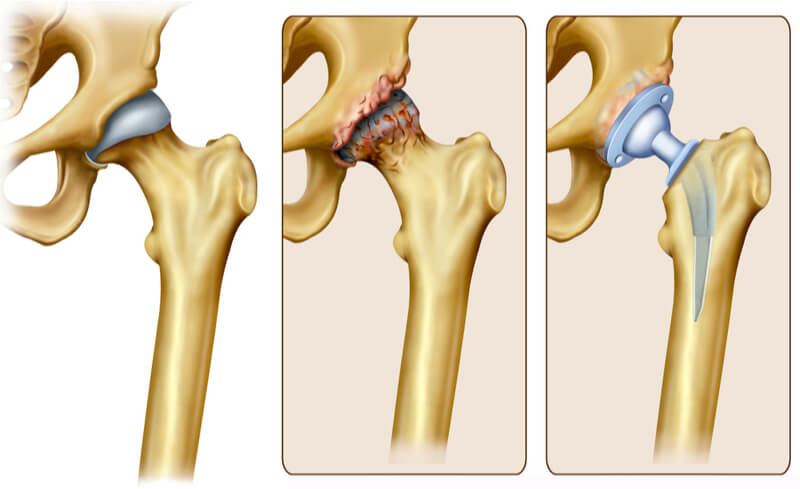
In the acetabulum (cup side), the worn-out cartilage is removed using a reamer and a titanium cup is put in its place. This is done under X-ray guidance to ensure that the size and position of the cup are appropriate. This ensures that patients have good mobility of their hip, low risk of dislocation and facilitates longevity of the hip implants in general. The surface of the titanium cup in contact with the acetabular bone is actual rough and covered in GRIPTION coatings. This porous coating technology allows stable fixation of the cup without the use of cement. The femur bone is then prepared to receive the femur implant. These femur implants come in various sizes and specifications to accommodate the large variety of femur bone shapes and sizes. In patients with normal strong bone, femur implants are inserted and impacted into the canal of femur bone till it achieves a stable position and fixation without the use of cement. These implants are coated with hydroxyapatite (HA) which allows its biological integration with the femur bone. For older patients or those with osteoporotic bone, femur implants may be inserted and stabilised by cement to prevent fractures of the femur bone itself. Once these implants are in position, either a ceramic or metal femoral head is inserted before the orthopaedic surgeon reduces the hip. All movements of the hip are tested and stress in all directions to mimic all the usual daily movements that patients require of their hip and to ensure that the hip joint is stable and will not dislocate.
The femur bone is then prepared to receive the femur implant. These femur implants come in various sizes and specifications to accommodate the large variety of femur bone shapes and sizes. In patients with normal strong bone, femur implants are inserted and impacted into the canal of femur bone till it achieves a stable position and fixation without the use of cement. These implants are coated with hydroxyapatite (HA) which allows its biological integration with the femur bone. For older patients or those with osteoporotic bone, femur implants may be inserted and stabilised by cement to prevent fractures of the femur bone itself. Once these implants are in position, either a ceramic or metal femoral head is inserted before the orthopaedic surgeon reduces the hip. All movements of the hip are tested and stress in all directions to mimic all the usual daily movements that patients require of their hip and to ensure that the hip joint is stable and will not dislocate.
Once the hip stability is found to be satisfactory, the trial implants are replaced with the actual implants. The wound is then washed with antiseptic solution and the wound is closed with sutures.
Dr Mizan also uses X-rays during surgery to ensure the following:
- All implants (acetabular and femur components) are the appropriate size
- All implants are inserted and stabilised in optimal positions to allow good and stable hip movements
- Both the operated and unoperated legs are of equal or near equal length after the procedure
- There are no fractures around the acetabulum or femur bone.
The use of intra-operative x-rays are possible during the direct anterior approach total hip replacement as patients are lying on their backs in a supine position. X-ray images are not as accurate if they are taken while patients are lying on their sides. Having intra-operative x-rays takes the guess work out of hip replacement surgery and there will not be surprises waiting after surgery is completed.
How does your surgeon enter the hip joint?
There are several ways to enter the hip joint before a hip replacement procedure can be performed. Traditional approaches include the posterior as well as the lateral approach. In these two techniques, patients lie on their sides during the surgery and muscles around the hip are split, cut or detached from bone to allow surgeon access into the hip joint.
With the posterior approach, there is a significant risk of the implants dislocating if patients squat or cross their legs. This is because the stabilising structures at the back of the hip (capsule and muscles) are compromised during surgery. These same structures are stressed when patients squat or cross their legs.
During the lateral approach to the hip, the side muscles of the hip (abductor muscles) are split and detached from the greater trochanter bone. Poor healing of these compromised muscles and tendons may lead to an abnormal walking (Trendelenberg) gait after surgery.
Pre-operative preparation
As the saying goes, ‘SAFETY FIRST’! All my patients above the age of 40 will require pre-operative assessments to ensure that they are fit enough for the surgery. Standard blood tests, chest x-rays and ECGs are done to ensure there are no underlying serious heart or lung conditions that may have been missed before. Blood tests ensure that patients have enough haemoglobin or red blood cells and normal kidney function to have surgery safely. Some patients who have underlying medication conditions may need to see a cardiologist or another specialist first before their planned surgery.
Medication
Most total hip replacement (THR) patients who undergo this procedure through the direct anterior approach (DAA) are admitted in hospital for one or two nights. They are given simple analgesia to help control their pain and allow them to do early physiotherapy and mobilisation. These medications include anti-inflammatory medication, paracetamol and muscle relaxants. Morphine-based medications are usually not required for the muscle-sparring DAA technique.
They are also given some antibiotics before and after their surgery to prevent any infection from setting in. Most of my patients do not require medication to prevent deep vein thrombosis (DVT) due to the DAA technique of doing the THR as well as early ambulation associated with this procedure. If patients are at risk of DVT, some medication (Clexane) may be given under the skin as well as compression stockings to prevent them from happening.
If you were previously on certain long-term medication before surgery, this may be started after surgery if they were previously stopped. Anti-platelet medication such as Aspirin or Plavix may be restarted at their regular dose the day after surgery. Other medications for hypertension or diabetes may also be restarted after surgery.
Physiotherapy
Physiotherapy and rehabilitation begin on the day of the surgery itself. For patients who have surgery in the morning, they are allowed to have their lunch when they return to their hospital suites before starting to walk in the mid-afternoon. We start off our patients by marching on the spot and walking using a frame. Once they have completed this, they may then use a walking stick to walk themselves around their suites or along the corridor of the ward. A physiotherapist will be at hand to assist patients when they are walking. The following day, patients start walking up and down stairs before they are deemed safe to return home. Most patients leave the hospital using a walking stick and will require them for a week or two. They may start to drive at two weeks once they have come off their walking aid .They are also allowed to squat, kneel and cross their legs as much as their flexibility and leg strength allows.
Wound management
The waterproof dressing over your groin wound may be changed upon discharge as they may be stained. The dressing may be changed between 5 to 7 days later and may be left exposed at the 2 week mark. The skin sutures do not need to be removed after your surgery as they self-dissolve.
After a Hip Replacement Procedure
Patients are prescribed with simple painkillers after surgery as no muscles are cut. A brief rehabilitation session with a physiotherapist to regain the use of the muscles may also be arranged on the same day as the surgery. This also helps to maintain muscle strength and improve their personal confidence.
After a second physiotherapy session the morning after, patients often leave the hospital after just one night’s stay.

Hip Replacement - after discharge from Hospital
Moving around
Dr Mizan encourages his patients to walk and move around as much as possible after surgery. This allows muscles to maintain their strength and flexibility. It also prevents scarring around the wound. The walking stick is there to help with your balance during the first few days. Once you have gained enough confidence walking, the stick may be left at home. Patients are also allowed to sit on normal chairs or toilet bowls. As the swelling around the hip muscles reduce, they will be able to cross their legs, kneel and squat better.
Medication
You would have been discharged from hospital with some medication to take for pain. This medication is there to help you move around comfortably and facilitate your rehabilitation. The medication given may be taken as required during different times of the day.
Anti-inflammatory medication such as Arcoxia is given to reduce pain and swelling in your hip. These medications are not addictive and are usually only taken for a few weeks. Muscle relaxants such as Anarex may be taken several times a day to reduce the stress on your muscles. Antibiotics are usually not required after discharge from hospital.
Precautions after total hip replacement surgery
With the DAA technique of THR surgery, the posterior structures of your hip are kept intact and are not compromised. As such, patients are allowed to squat, kneel and cross their legs should they choose to. The risk of posterior hip dislocation with regular daily activities is negligible.
Patients are allowed to cross their legsafter surgery.
Patients are however advised not to allow their operated leg to be pulled forcefully such as during bungee jumps and aggressive forms of massage and manipulation. This may cause their hip to dislocate.
Leg traction is not allowed.
Preparing the home
Patients are advised to consider their home environment before they have surgery. While they are allowed to walk up and down stairs, they may choose to sleep in the bedroom on a lower level rather than on level 3 of their home. You should consider adding the following safety items to your home.
Place a comfortable chair in every room, including the kitchen and bathroom.
Install a rail or handle in the shower or along stairs to give you added safety.
Use slip-proof or gripping mats in the bathroom and around the house.
Diet
Foods high in proteins and vitamins like calcium are good for your post-surgery diet. Examples include fish, skinless poultry, eggs, fruits, and vegetables. Carbohydrates are also important to give you energy to move about and attend your physiotherapy sessions. There are no diet restrictions associated with hip replacement surgery. Patients are advised to comply with their usual diet restrictions associated with diabetes, gout and other medical conditions.
How much does a Hip Replacement cost in Singapore?
The price for hip replacements in Singapore ranges from $10,000 for subsidised patients in government hospitals to about $40,000 in Private hospitals. The orthopaedic clinic that you visit will give you a breakdown of the total cost. This includes the following:
- Facilities and hospital fees (largest expense)
- Surgeon fees (amount dictated by Ministry of Health or Insurance Companies)
- Anaesthetic fees ((amount dictated by Ministry of Health or Insurance Companies)
- Implant costs
- Additional measures post-op i.e. medication, dressings, walking stick
There are various forms of medical insurance used in Singapore (Personal vs Corporate, Local vs Foreign, Elective vs Accident). Some insurance policies will require patients to co-pay a certain amount for their treatment. As such, pre-operative financial counselling is an important process that we adhere to to ensure that you receive your medical treatment with peace of mind and can focus on your recovery.
Speak to our orthopaedic surgeon Dr Mizan Marican today to assess your hip conditions and understand more about how we can help you achieve a better quality of life.
Is it alright to walk around with a sprained ankle?
This depends on the sprain's severity and what treatment has been rendered for the injury. Your doctor may advise you to only put minimal weight on your ankle while it is still recovering from the injury. Excessive walking may lead to more pain and swelling if the injury is stressed too early on.
How do I know if my ankle sprain is serious?
The nature of the initial accident or injury will provide a good idea about how fast it may recover. A serious injury is characterized by severe pain, swelling, and recurrent sprains despite efforts to support and treat it. If you are experiencing these, the soonest visit to the specialist is highly advised.
Can I claim insurance for my ankle injury?
Ankle sprains and injuries are insurance claimable. We do advise our patients to check with their personal or corporate insurance plans and representatives. We are also able to help them with this if required.
What should I do immediately after an ankle sprain while waiting for my appointment and treatment?
Timely self-care with rest, icing, compression, and elevation are important to manage the initial pain and swelling around the ankle. Anti-inflammatory medication will further reduce the pain and swelling that you may be experiencing.
I have more questions, how can I speak to a doctor?
Please call us at +65 6733 4565 (during office hours), or drop us a text or WhatsApp message at +65 9766 4565. We will reply to your queries as soon as we get them. You may also call to make an appointment to see Dr. Mizan for your ankle injury.