When to Consider Hip Preservation and Total Hip Replacement
Hip preservation techniques are aimed at rectifying and treating injuries around the hip and prevent the need for a total hip replacement. If the hip condition is too far advanced, a hip replacement surgery may be required to ensure you continue to live a healthy and active life.
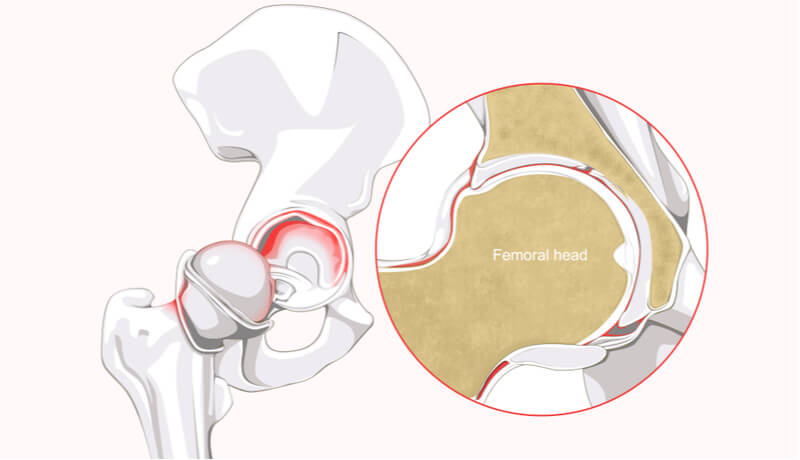
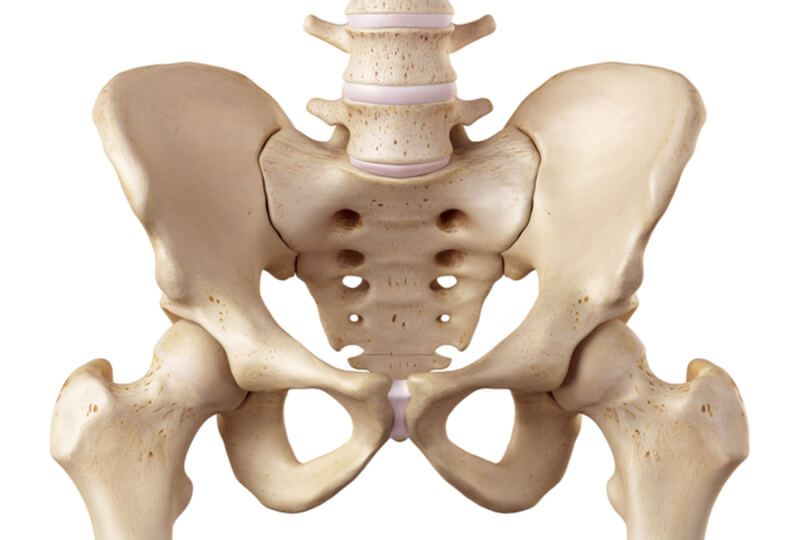
Hip anatomy and common hip conditions
The hip is a ball and socket joint that is lined with cartilage and a labrum. These two important structures ensure painless and smooth movement of the hip as we go about our daily activities. There are many degenerative and developmental conditions which may cause a breakdown of these shock absorbers of the hip that can bring about pain and stiffness. If left untreated, simple injuries of the hip may escalate into advanced arthritis (degenerative wear and tear).
The labrum is a thin cartilage around the edges of the socket (acetabulum). It helps to distribute lubricating (synovial) fluid around the hip to keep it healthy and smooth. Trauma and injury may cause a labrum tear. This may bring about pain in the groin, accompanied by clicking or clunking sensations. If left untreated, the labral tear may get bigger and lose its ability to protect the hip against arthritis. Physiotherapy is instituted after surgery to help with flexibility of the hip and ensure a satisfactory recovery.
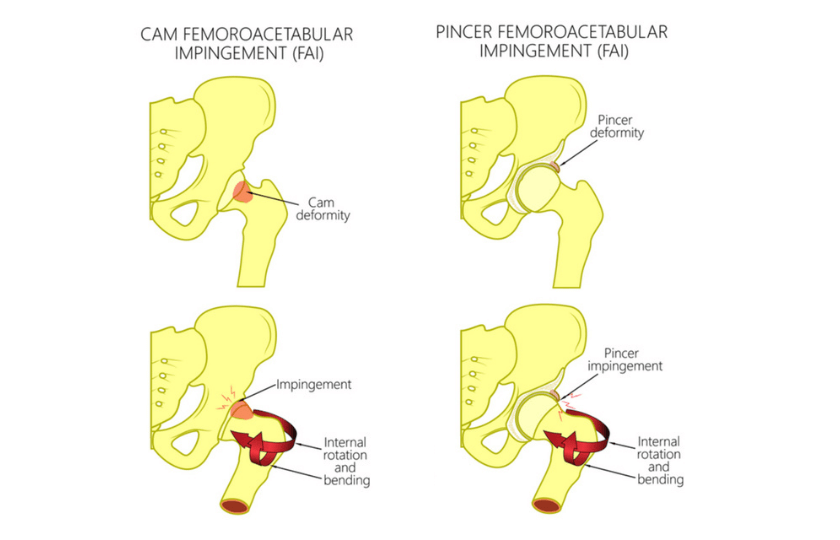
Femoral acetabular impingement (FAI)
Femoral acetabular impingement (FAI) is a developmental condition where there is excess bone along the edges of the acetabulum, at the junction of the femoral head and neck or both. It’s like having pebble in your shoe which keeps irritating the sole of your foot until you get a severe abrasion.
FAI can cause your hip labrum to tear and hip cartilage to wear out. Your hip condition may progress to arthritis if this is left unchecked. MRI scans may be done several months after your surgery to ensure that your hip cartilage and labrum are in good order. Physiotherapy is an important part of the recovery process to ensure you maintain strength and flexibility in your hips and lower limbs.
Avascular necrosis (AVN)
Avascular necrosis (AVN) is a condition where the blood supply to the femoral head bone in the hip is disrupted. This may be due to a variety of causes including excessive alcohol intake, long term steroid use and chemotherapy medications. AVN leads to a collapse of the femoral head and eventual arthritis.
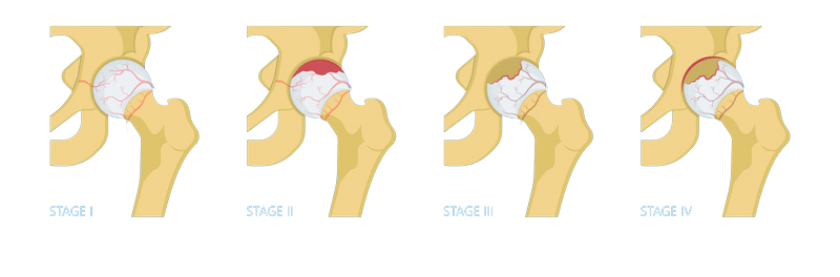 The various stages of AVN. Hip preservation surgery is amenable for Stages 1 and 2.
The various stages of AVN. Hip preservation surgery is amenable for Stages 1 and 2.
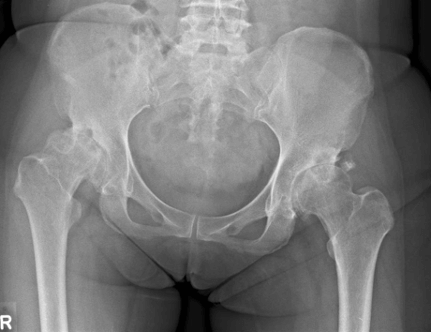
Hip arthritis
Hip arthritis is a condition where there is degenerative wear and tear or thinning of the hip cartilage. The protective and shock-absorbing functions of the cartilage are lost, leading to severe pressure to the hip joint itself. Patients with hip arthritis often experience debilitating hip pain, stiffness and walk with a limp.
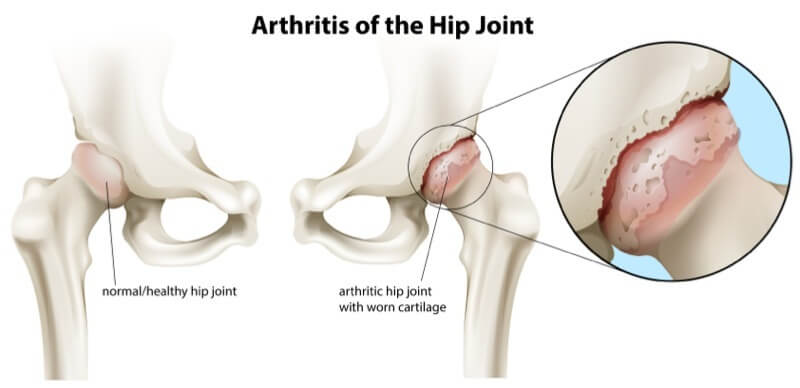 Hip arthritis with the ball and socket joint worn out.
Hip arthritis with the ball and socket joint worn out.
Hip preservation surgery
There are now arthroscopic (key hole) techniques to preserve the hip and prevent or delay the need for a formal hip replacement. Labral tears are repaired and stitched back to the rip of the acetabulum using long and narrow instruments which are inserted through small 1-2cm skin incisions around the hip (arthroscopic labral repair).
For FAI
FAI injuries are also managed by this same technique where abnormal fragments of bone around the acetabulum and femoral neck are removed using burr and shaver instruments (arthroscopic pincer and CAM resection).
Key hole techniques help reduce the risk of infection and collateral damage to other structures in the hip. Your surgeon will have an excellent view in the hip as these minimally invasive techniques are associated with minimal blood loss. We have a formal rehabilitation program that patients embark on after their surgery to optimise their recovery.
For AVN
AVN is associated with an increased pressure in the femoral head. This prevents blood flow to it and causes it to eventually collapse. It is important to seek early treatment for this as hip preservation techniques can only be used in its early stages (Stage I and II).
In these instances, a small 2cm incision is made on the side of the hip. Small wires are then advanced into the femoral head itself to decompress the pressure within the bone (core decompression). This encourages blood flow to return to the bone and help with its healing. We also improve the biology of bone healing by including bone graft into the femoral head. In combination, these techniques help to reduce bone pressure and improve bone healing mechanisms within the femoral head.
Serial X-rays are done several weeks and months after surgery to ensure that the femoral head in the hip maintains its spherical shape and continues to heal. We also ensure that our patients refrain from excessive drinking and steroid use to prevent deterioration of their condition.
For hip arthritis
In the early stages of hip arthritis, hip preservation techniques include intra-articular injections into the hip joint itself. Single and multiple doses of hyaluronic acid have been shown to improve hip pain and function as a result of hip arthritis.
 Injection into the hip joint as a form of hip preservation technique.
Injection into the hip joint as a form of hip preservation technique.
Hip Replacement Surgery
This surgical technique involves removing the worn out parts of the hip and replacing them with specialised implants. The aim of this surgery is for patients to return to their active lifestyle and enjoy continued employment, sports, holidays or simply go about their daily activities without hip pain and disability.
Your orthopaedic surgeon will analyse your latest X-ray or MRI scans of the hip and conclude that the cartilage (shock absorber) and labrum (stabiliser) of the hip are worn out. This leads to very rough and painful movements in your hip. At this point, you might already be experiencing the following symptoms:
- Deep-seated hip pain and stiffness
- Walking with a limp or waddling gait (your body swinging from side to side when walking)
- Having to use a walking aid
- Difficulty putting on clothes and socks
- Difficulty cutting your toe nails
- Difficulty with daily activities like climbing stairs
- Pain killers becoming less effective
The hip replacement surgery takes about two and a half hours. The 10cm skin incision is located in your groin at the front of your hip. The muscles are pushed aside so that we may access the hip. The worn-out bones and cartilage are carefully removed using specialised equipment, and implants are then put in their place which best fit your bone shape and size.
During surgery, your orthopaedic surgeon will move your hip about to simulate daily activities such as sitting on a chair, squatting and sleeping on your side. This is to ensure your hip is stable and does not dislocate when you go about your daily activities. We also ensure both legs are of the same length by clinical measurement and the use of X-rays.
My patients are able to walk on the same day as their surgery. Under the watchful eye of our physiotherapist, my patients will start to walk with the use of a walking frame and stick around their hospital room. The minimally invasive techniques allow accelerated walking and physiotherapy after surgery. My patients are discharged the day after surgery once they are deemed to be safe on their feet. I always encourage my patients to walk as much as possible after their surgery.
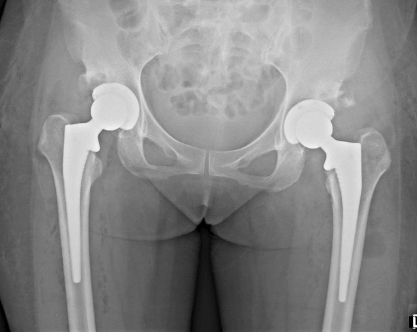
Hip replacement surgery performed in a patient with arthritis affecting both hips.
They are allowed to return to their favourite sporting pastimes such as brisk walking, swimming, tennis and golf. My patients are also allowed to squat and kneel after their hip replacement surgery. To improve their confidence, I will guide them to perform these movements and exercises in the safety and comfort of my clinic room in the presence of their family members or caregivers.
I often explain to patients and their loved ones that a hip replacement is often the start of a new and refreshing phase of their life. This is especially since so many of them would have experienced years of hip pain and crippling disability. We encourage our patients to live an active and healthy life after hip replacement surgery.
Conclusion
Please seek professional orthopaedic help if you experience any hip, knee or back pain. An early assessment and clinical examination accompanied with appropriate imaging (X-rays and/or MRI scans) will allow the early diagnosis of injuries and conditions of the hip. In these instances, hip preservation techniques may be instituted to get you back to your active life. If the hip injury and degeneration is too far advanced, a hip replacement procedure is an ideal option to manage your chronic pain and significantly improve your quality of life.
Schedule a consultation with our consultant orthopaedic surgeon Dr Mizan Marican to find out the right treatment for your hip condition.
Is it alright to walk around with a sprained ankle?
This depends on the sprain's severity and what treatment has been rendered for the injury. Your doctor may advise you to only put minimal weight on your ankle while it is still recovering from the injury. Excessive walking may lead to more pain and swelling if the injury is stressed too early on.
How do I know if my ankle sprain is serious?
The nature of the initial accident or injury will provide a good idea about how fast it may recover. A serious injury is characterized by severe pain, swelling, and recurrent sprains despite efforts to support and treat it. If you are experiencing these, the soonest visit to the specialist is highly advised.
Can I claim insurance for my ankle injury?
Ankle sprains and injuries are insurance claimable. We do advise our patients to check with their personal or corporate insurance plans and representatives. We are also able to help them with this if required.
What should I do immediately after an ankle sprain while waiting for my appointment and treatment?
Timely self-care with rest, icing, compression, and elevation are important to manage the initial pain and swelling around the ankle. Anti-inflammatory medication will further reduce the pain and swelling that you may be experiencing.
I have more questions, how can I speak to a doctor?
Please call us at +65 6733 4565 (during office hours), or drop us a text or WhatsApp message at +65 9766 4565. We will reply to your queries as soon as we get them. You may also call to make an appointment to see Dr. Mizan for your ankle injury.